Mitigating pregnancy risks with a comprehensive care team
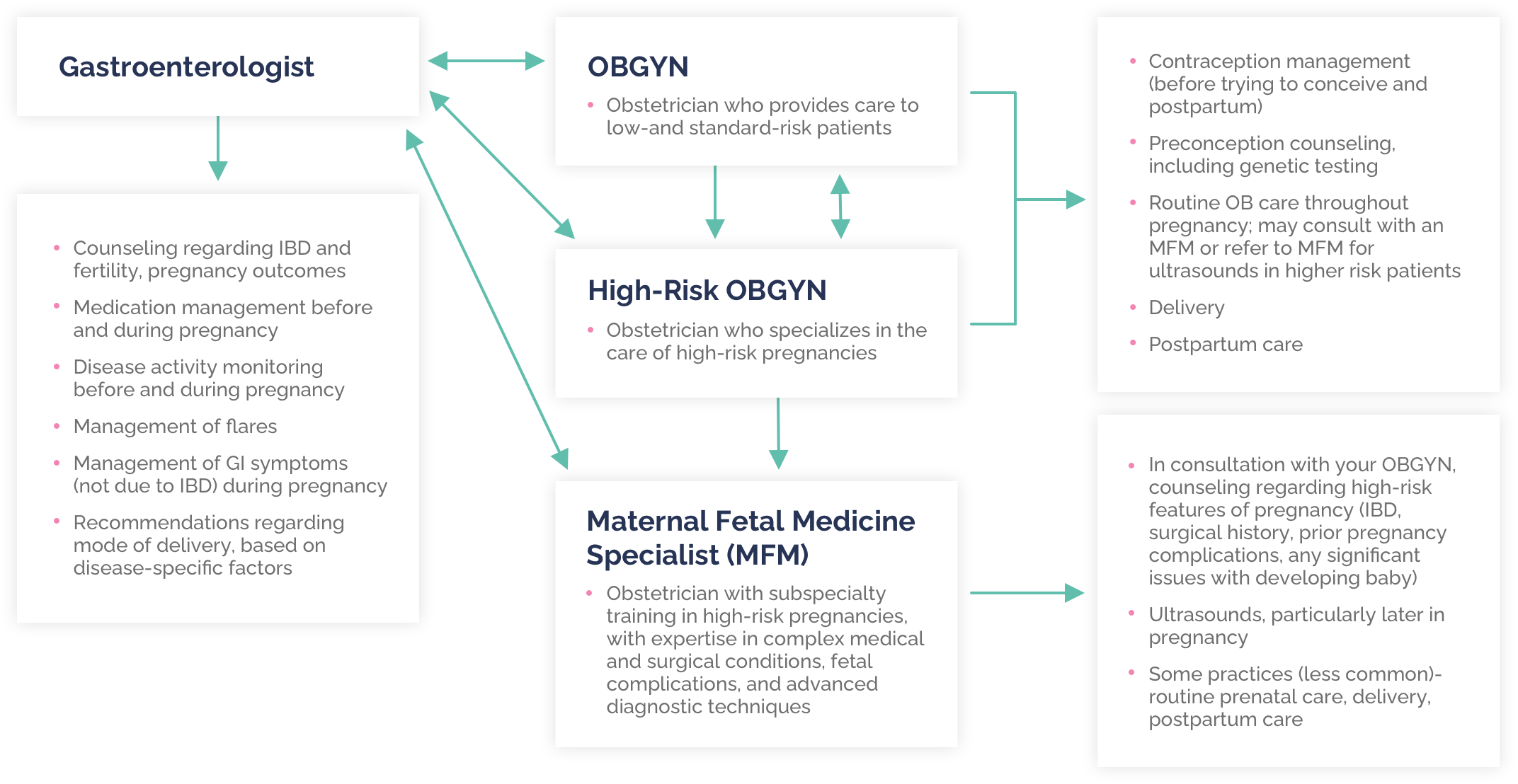
Most women with IBD have healthy, uncomplicated pregnancies, especially when their disease state is optimized before conception. In fact, several studies have shown that women with IBD who go into pregnancy in a deep remission are more likely to stay in remission while pregnant. However, there are potential risks associated with IBD and pregnancy. That's why it's important to approach your pregnancy with the care of several doctors—not just your Ob/Gyn. Working with a high risk Ob/Gyn, gastroenterologist and maternal-fetal medicine specialist (MFM) can provide you with different aspects of care—optimizing the health of you and your baby before, during and after pregnancy. Additionally, if you have a history of IBD surgery, your colorectal surgeon should be involved in your pregnancy care team. Lastly, a nutritionist may be helpful prior to and during pregnancy.
Risks associated with active IBD
Active IBD before pregnancy may lead to significant inflammation in the pelvis. This inflammation can also affect the body's neighboring uterus, fallopian tubes and ovaries, which are of utmost importance during conception and pregnancy. Left unchecked, it can even lead to the formation of scar tissue, which can make conceiving difficult.
Once pregnant, inflammation in this area can significantly impact the health of the pregnancy. It can increase the risk of miscarriage in the first trimester and later lead to your water breaking early, preterm delivery, and, in some cases, stillbirth. Inflammation can also result in low birth weights upon delivery due to restricted nutrition delivery to the fetus during the pregnancy.
Ways to reduce risk
These potential complications can be greatly reduced by ensuring your IBD is in remission when trying to conceive and keeping your symptoms in control throughout your pregnancy. Data shows that approximately two-thirds of women who are in remission pre-pregnancy will stay in remission throughout their pregnancy. Conversely, women with active disease are likely to have continued flare-ups during pregnancy. These women are at the highest risk for the pregnancy complications described above. Learn more about controlling your disease during pregnancy here.
How to prepare
Meeting with an MFM specialist before trying to become pregnant is the best way to optimize disease control and ensure remission during your pregnancy. If needed, this type of doctor can work with your IBD specialist to adjust your medication to one that is safe throughout pregnancy, since discontinuation of certain medications abruptly (such as when you discover you're pregnant) can be associated with an IBD flare.
Once pregnant, your MFM specialist will be able to help you address any symptoms or concerns throughout your pregnancy. Starting in your third trimester, this doctor will also be able to perform serial fetal growth ultrasounds and additional fetal testing to ensure that your baby is growing correctly. At this time, she can also help you determine the healthiest mode of delivery for you and your baby. Learn more about IBD and delivery, here.
Takeaway message
There are several risks or complications that can take place during pregnancy for women with uncontrolled IBD symptoms. However, by treating and maintaining your IBD before becoming pregnant, you can prevent many of these risks from becoming concerns. By working with an MFM specialist and gastroenterologist, in addition to your Ob/Gyn, you'll be able to further reduce your risk of complications and make a plan for the healthiest pregnancy possible.
